Healthcare workers often face accidents/occupational injuries from which they get accidental exposure to blood born infections e.g. HIV, Hepatitis B and C. When there is potential exposure to HIV, HIV infection can be prevented by taking Post Exposure Prophylaxis (PEP) with antiretroviral drugs as soon as possible (Ideally within 72 hours).
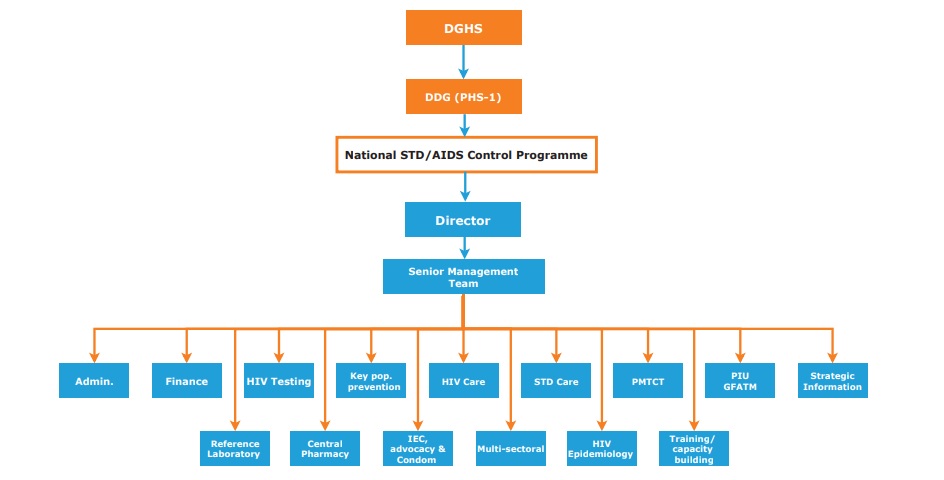
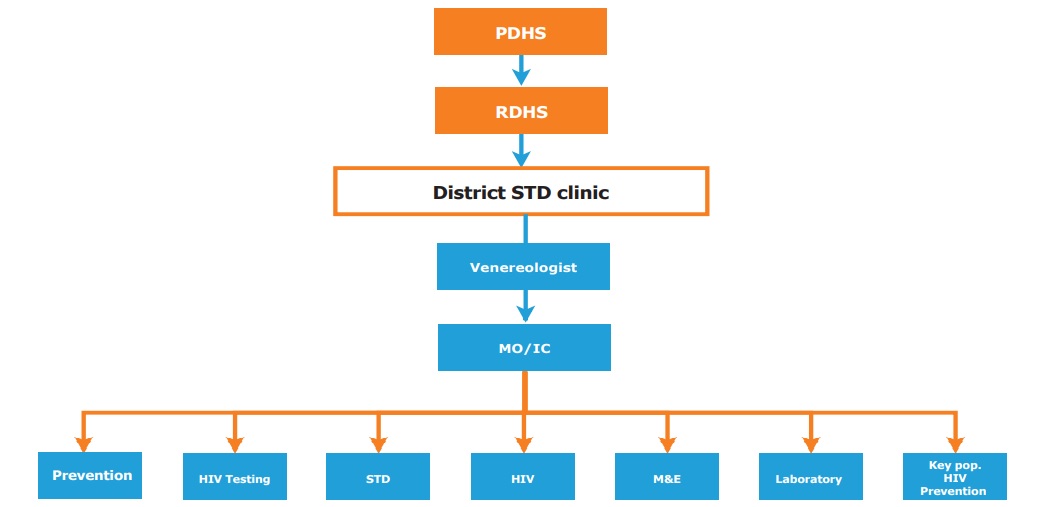
NSACP has made PEP available in all districts island-wide through its 41 islandwide clinic network and provides starter packs of ART to identified 24-hour functioning units in all 25 districts.
What are the high-risk exposures?
Prick injuries/Cuts/Mucous membrane exposure(Splashes) with exposure to the following body fluids.
- Blood and products-serum/plasma etc
- CSF
- Spermatic fluid
- Vaginal secretions
- Cerebrospinal fluid
- Synovial, pleural, peritoneal, pericardial fluid
- Amniotic fluid
- Other body fluids contaminated with visible blood
Exposure to tears, sweat, urine, faeces or saliva is considered risk-free unless they are visibly contaminated with blood.

Risk of HIV after a sudden prick injury from a random patient from the community?
< 0.3%.
The risk depends on
- Source should be HIV positive with a high Viral load in the source patient with HIV. (Acute HIV infection or terminal HIV-related illness).
- Depth of the injury.
- Visible blood on the device which caused the injury.
- Injury with a needle which had been placed in a source patient’s artery or vein.
What to do after a potential exposure?
- Wash liberally with soap and water without scrubbing.
- Don’t use antiseptics (Surgical spirit or Betadine) and skin washes.
- Don’t squeeze or suck the wound site
- Irrigate the exposed mucous membranes, including conjunctivae copiously with water, before and after removing any contact lenses.
- Inform the hospital infection control nurse and update the register.
- Get the source patient’s consent for testing for HIV, Hepatitis B and Hepatitis C.
- Take 3 cc blood of the patient to a plain bottle for HIV and come to the nearest STD clinic as soon as possible, or call the STD clinic for more details.


What is done at the STD clinic?
- A risk assessment to decide on the appropriateness of starting PEP for HIV.
- HIV testing- A rapid HIV test and an HIV ELISA test will be done on the source patient’s blood sample.
- Baseline investigations will be done on the HCW- HIV ELISA, Renal and liver function tests, and Urine HCG test if applicable.
- If PEP is indicated following the risk assessment, PEP will be provided to be taken for 28 days.
- PEP has to be taken as prescribed and regular follow-up is important. HIV ELISA will be done in 6 weeks and 12 weeks in the follow-up.
What to do if the exposure occurred outside clinic hours?
- Initial assessment of exposure by a designated medical officer in the institution for the purpose.
- Initiate the Starter pack* as early as possible (preferably within 2 hours) if eligible.
- Contact Microbiologist/ Virologist/ On call MO Microbiology for Hep B / Hep C.
- Refer the health care worker to the closest Venereologist or District MO STD on the following working day for further management.
- Inform Infection Control Unit as early as possible.

*Starter pack is antiretroviral medication for the post-exposure prophylaxis for 5 days Three drugs- (Tenofovir+Emtricitabine) Raltegravir/Efvavirnze/Dolutegravir etc.